Digital health on Main Street: Revolutionizing rural America with telehealth and consumerization
The integration of digital health and the growing consumerization of services are reshaping the health care landscape, especially in rural America. Just as online banking and shopping have revolutionized daily activities, telehealth is transforming health care delivery in underserved communities. Many of the reasons rural hospitals have been historically disadvantaged are central to the argument that these institutions are uniquely positioned to capitalize on digital health innovations.
The consumerization of health care
In the modern era, consumers expect seamless, on-demand experiences in all aspects of life, including health care. The rise of telehealth mirrors the shift seen in other industries like banking and retail, where convenience and accessibility are paramount. COVID-19 was a prime example of our resilience leading us to leverage online platforms to purchase goods, catch up with distant family, or seek health care services. In rural communities where distance can limit access, telehealth provides an opportunity to bridge the gap in health care services, ensuring residents receive timely, quality care without the need to travel long distances.
Telehealth as a health care utilization concept
Telehealth is more than just a technological innovation – it is a fundamental shift in how health care resources are utilized. By enabling virtual consultations and remote monitoring, telehealth optimizes the role of health care professionals, ensuring their expertise is accessible across diverse geographical areas. With 15 percent of Americans living in rural areas but only 10 percent of doctors practicing in these communities, telehealth can allow health care providers to deploy resources where they are most needed. This enhances care delivery in remote areas by breaking down geographical barriers to ensure rural populations have access to specialized care.
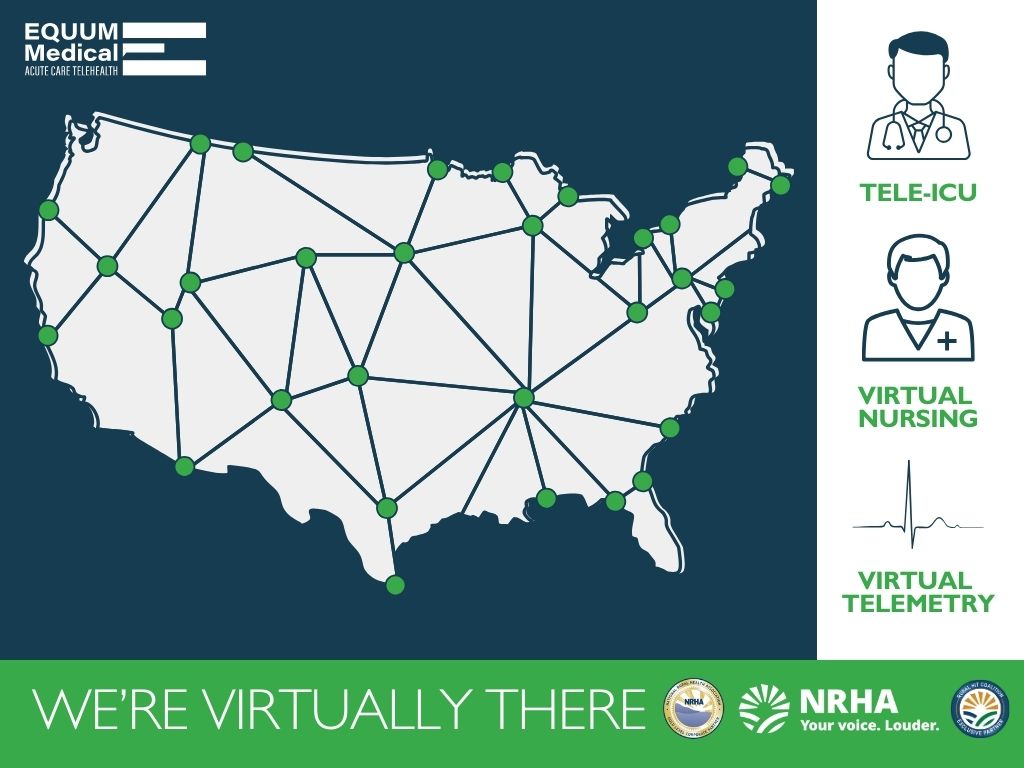 |
Beyond access, “time to care” is a crucial factor in keeping a patient at a critical access hospital. Telehealth reduces the need for patients to travel long distances for essential health care services, with the expansion of multi-specialty applications like cardiology, nephrology, and infectious disease improving patient outcomes and reducing the burden on local health care facilities. Virtual consultations enable health care professionals to manage their time more efficiently and enhance the overall patient experience, particularly in rural areas where health care facilities may be limited.
Design for the future: Go virtual first
One of the key advantages of telehealth is its scalability. By leveraging digital platforms, health care providers can reach a larger population without significant infrastructure investments. This scalability ensures that even remote populations have access to timely and quality care, improving the overall health care delivery system. Following an initial foray into telehealth, organizational leadership often shift to a "virtual first" mindset where each discussion begins with the question of a virtual implementation, opening new dimensions of accessible care.
Final thoughts
The intersection of digital health and consumerization is transforming rural health care. By embracing telehealth, rural hospitals can overcome geographic and resource limitations, providing high-quality care to their communities. This revolution in health care delivery ensures that rural populations receive the care they need when they need it without the constraints of traditional health care models.
Telehealth finds the perfect home in rural health care due to the vast geography and lack of specialist resources. The urgency to innovate, openness to collaborate, and ability to leverage digital health are essential for transforming health care in rural America. This approach ensures rural hospitals are not left behind but are instead at the forefront of health care innovation.
NRHA adapted the above piece from EQUUM Medical Acute Care Telehealth, a trusted NRHA partner, for publication within the Association’s Rural Health Voices blog.
 | About the author: Corey Scurlock, MD, is the founder and CEO of Equum Medical. Dr. Scurlock is an intensive care specialist with a deep background in acute care telemedicine, starting his first program in 2011. As the CEO and founder of Equum, Dr. Scurlock has grown it from its original singular hospital and service capabilities to over 100 hospitals with a footprint of purpose-built, digitally-enabled clinical services across the hospital acute care continuum and post-acute facilities. |
